In the realm of vision, few conditions are as impactful as macular degeneration, especially among those over 50. This disorder targets the macula, the eye’s center, blurring and altering your central vision.
As the world’s sights become hazier for those affected by macular degeneration, understanding this ailment is crucial. This guide delves into the intricacies of macular degeneration, offering insights and highlighting supportive measures for maintaining eye health.
What Is Macular Degeneration?
Macular degeneration is a progressive eye condition that primarily affects the central area of the retina, known as the macula. Responsible for sharp, clear central vision, the macula deteriorates in those with this condition, leading to blurred or distorted vision.
Often associated with aging, the most common form is age-related macular degeneration (AMD), which has two types: wet and dry. While dry AMD is characterized by the thinning of the macula, wet AMD involves the growth of abnormal blood vessels beneath the retina.
The condition can make tasks like reading, driving, and recognising faces challenging. Although there’s no cure, treatments and lifestyle changes can help manage its progression and maintain eye health.
Understanding the Macula
At the heart of our visual acuity lies the macula, a pivotal component of the retina. To truly grasp the intricacies of macular degeneration, we must first delve into understanding the macula itself.
Anatomy of the eye
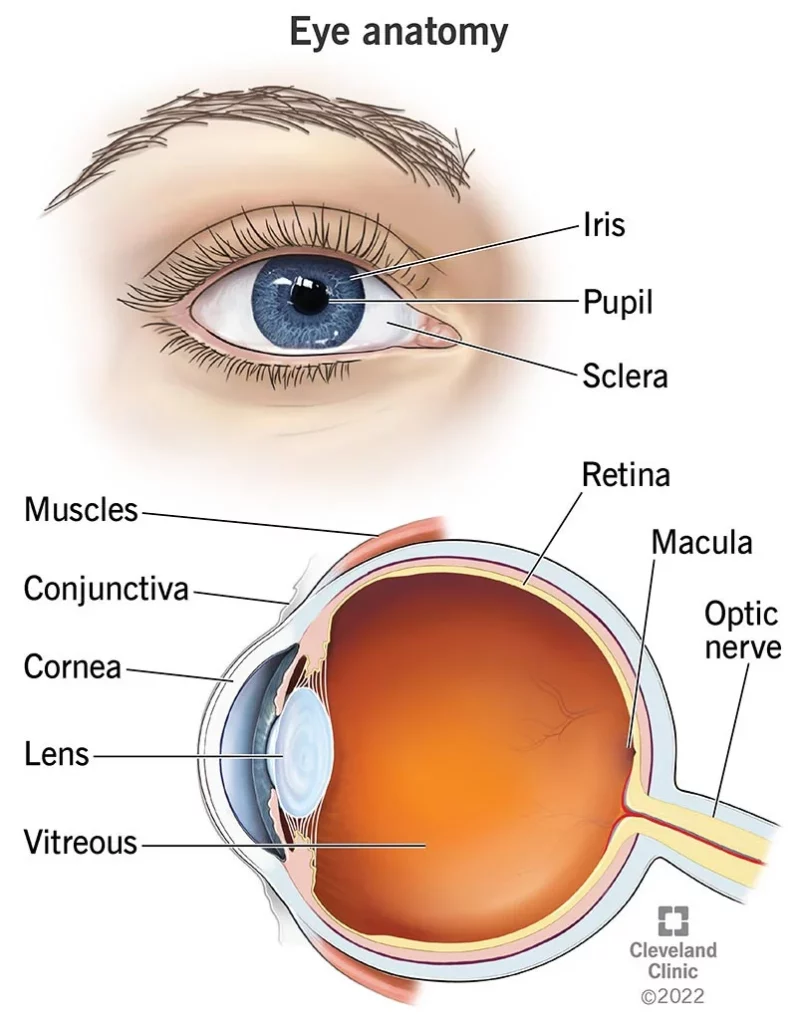
The human eye is a marvel of biological engineering, seamlessly translating light into the images we perceive.
- The Eyeball: The eye can be envisioned as a slightly asymmetrical ball, filled with fluids that maintain its shape.
- Cornea: This is the transparent front layer of the eye. It refracts (bends) light as it enters the eye.
- Iris: The coloured part of the eye, which controls the size of the pupil. The iris adjusts the pupil’s size to regulate the amount of light entering the eye.
- Pupil: The dark central opening in the iris that adjusts in size and controls the amount of light entering the eye.
- Lens: Located right behind the pupil, it further focuses light onto the retina. It’s elastic and changes shape (accommodates) to help focus objects at various distances.
- Vitreous Humour: A clear, jelly-like substance that fills the middle part of the eyeball. It helps maintain the eye’s shape and allows light to pass through to the retina.
- Retina: This is the light-sensitive layer at the back of the eye. It contains cells called photoreceptors (rods and cones) that capture light and convert it into electrical signals.
- Macula: The macula is a small central area of the retina. It is rich in cones and is responsible for our sharp, central vision. This is the part of the eye most affected by macular degeneration.
- Optic Nerve: The nerve that connects the eye to the brain. It transmits the electrical signals from the retina to the brain, where these signals are interpreted as visual images.
- Choroid: A layer rich in blood vessels, located between the retina and the white of the eye (sclera). It provides oxygen and nutrients to the retina.
- Sclera: The white, outer protective layer of the eye. It is tough and maintains the shape of the eye.
The macula & its function
Situated at the centre of the retina is the macula. It’s a small, pigmented area measuring about 5.5 mm in diameter. While tiny, it plays a significant role in our vision due to its high concentration of photoreceptor cells, specifically the cone cells which are responsible for colour vision and the fine detail of what we see.
Unlike the rest of the retina, which provides peripheral vision, the macula focuses on the details. When you read, recognise faces, drive, or even thread a needle, you’re relying heavily on your macula.

Importance of the macula
Central Vision and Daily Life Implications: Without a healthy macula, tasks that require detailed vision become challenging. Reading, writing, recognising faces, and driving all rely on the macula’s capabilities. A damaged or degenerating macula can impede these daily functions, significantly affecting one’s quality of life.
Color Perception: The macula’s concentration of cone cells allows us to perceive a full spectrum of colors. When the macula is compromised, color perception can diminish.
Depth and Detail Perception: From discerning the texture of fabric to noticing the fine details in artwork, the macula provides the clarity and depth required.
Types of Macular Degeneration
There are several types of macular degeneration, each with distinct characteristics and causes.
Age-Related Macular Degeneration (AMD)
AMD is the most common form of macular degeneration, typically affecting older adults, leading to a gradual loss of central vision. It’s primarily categorized into two types: Dry and Wet.
Dry AMD
Dry AMD is the most prevalent form of the disease, affecting about 85-90% of individuals with AMD. It’s characterized by the thinning of the macula, which can lead to the formation of small yellow deposits called drusen beneath the retina. The presence of drusen is a primary hallmark of this condition.
Causes: The exact cause of Dry AMD isn’t fully understood. However, it is believed to be a result of aging and thinning of macular tissues, depositing of pigment in the macula, or a combination of both. Environmental factors, genetics, and lifestyle choices, like smoking, can also contribute to its development.
Wet AMD
Though less common, Wet AMD is more severe and progresses more rapidly than its dry counterpart. It’s marked by the growth of abnormal blood vessels from the choroid (a layer of blood vessels between the retina and the sclera) underneath the retina. These new blood vessels are fragile and prone to leaking blood and fluid.
Causes: The exact cause of the abnormal blood vessel growth in Wet AMD remains a topic of study. However, it’s known that these vessels leak fluid and blood, leading to scarring of the macula and rapid central vision loss. Factors that may increase the risk include genetics, smoking, and high blood pressure.
💡 Read more: Which Is Worse: Dry or Wet Macular Degeneration?

Juvenile Macular Degeneration
Distinct from AMD, juvenile macular degeneration is a group of inherited disorders that affect children and young adults. Unlike AMD, which is due to aging, these conditions are genetic and often become apparent in childhood or adolescence.
Types Of Juvenile Macular Degeneration:
- Stargardt’s disease: The most common form of juvenile macular degeneration, Stargardt’s disease, causes progressive vision loss, usually to the point of legal blindness.
- Best disease: Also known as vitelliform macular dystrophy, it affects the layer of the retina essential for sharp vision. Although vision loss is gradual, it can vary in severity.
- Juvenile retinoschisis: This rare genetic disorder causes a split or schism in the retina, leading to vision loss.
Causes: These conditions are primarily caused by mutations in specific genes. Children inherit the faulty gene from their parents, often even if the parents don’t show signs of macular degeneration themselves. Early detection and genetic counseling can be crucial for families with a history of these conditions.
Risk Factors and Causes of AMD
Macular degeneration, particularly the age-related form (AMD), is influenced by a combination of genetic, environmental, and lifestyle factors. Understanding these can provide a clearer perspective on preventive measures and potential interventions.

Age
Age stands as the primary risk factor. The likelihood of developing AMD increases significantly for those over the age of 50. The degenerative changes associated with aging tissues in the retina and macula enhance vulnerability.
Genetics
The role of heredity shouldn’t be understated. Individuals with a family history of AMD are at a heightened risk. There have been several genes identified that are associated with a higher likelihood of developing the condition.
Smoking
Smoking is not just detrimental to lung health but is also a significant risk factor for AMD. It is believed that smoking may reduce the protective antioxidants in the eye, making it more susceptible to damage from oxidative stress.
Obesity
Excessive body weight not only affects cardiovascular health but also stands as a risk factor for macular degeneration. Obesity can exacerbate other risk factors, and there’s a correlation between high body mass index (BMI) and AMD progression.
Other contributing factors to macular degeneration
1. High Blood Pressure
Chronic hypertension or high blood pressure, over time, can have adverse effects on the eye’s blood vessels, especially the tiny capillaries nourishing the retina and macula.
Impact: With prolonged hypertension, these vessels can become weak or damaged, restricting the flow of blood and essential nutrients to the retina. This deficiency might lead to the onset or exacerbation of AMD.
Prevention: Regular monitoring and controlling of blood pressure, through lifestyle changes or medication as advised by a doctor, can potentially delay or prevent the development of AMD.
2. Excessive Sun Exposure
The eyes, just like skin, are susceptible to damage from prolonged exposure to ultraviolet (UV) rays.
Impact: UV rays can accelerate damage to the retina, especially the macula, which might hasten the development of macular degeneration.
Prevention: Wearing sunglasses with UV protection, even on cloudy days, and a wide-brimmed hat can shield the eyes from direct sunlight, thereby decreasing the risk.
3. Diet
What you consume plays a significant role in overall health, including eye health.
Impact: Diets rich in saturated fats can potentially clog the tiny blood vessels in the retina. Simultaneously, a lack of essential nutrients like antioxidants and zinc can deprive the retina of vital nourishment, potentially increasing the risk of AMD.
Prevention: Consuming a balanced diet, rich in leafy greens, colorful fruits, and fish rich in omega-3 fatty acids can be beneficial. Supplements might also be recommended in certain cases.
4. Gender and Race
Demographics, including gender and race, play a role in the susceptibility to AMD.
Impact: Studies have shown that women have a higher likelihood of developing AMD than men. Additionally, Caucasians are more at risk than African-Americans or Hispanics/Latinos, possibly due to differences in pigmentation and genetic factors.
Prevention: While one cannot change their gender or race, being aware of heightened risks can motivate regular eye check-ups and early detection, which are crucial for managing AMD effectively.
Symptoms and diagnosis
Early detection of Age-Related Macular Degeneration (AMD) can significantly impact its management, potentially slowing down its progression and preserving vision. Recognizing the symptoms and understanding the diagnostic methods are crucial steps.
Early Symptoms
Understanding the onset of macular degeneration symptoms can be vital for timely intervention:
1. Blurred Vision
This is often the initial sign. Individuals might notice:
- A need for increased light when reading.
- Difficulty in recognizing faces from a distance.
- Text appearing hazier.
2. Distorted Vision
It might be subtle at first but can be identified when:
- Straight edges, such as door frames or lines on paper, appear wavy or bent.
- Patterns like tiles might seem misaligned.
3. Shadowed Vision
This can manifest as:
- A dark patch in the center of one’s view.
- An empty or ‘missing’ area when focusing on a specific spot.
4. Colour Changes
Colors might not appear as they used to. This change can be seen as:
- Colors appearing less bright or washed out.
- Difficulty distinguishing between shades of a particular color.
Progression of Symptoms
As ARMD advances, symptoms can intensify or expand:
- Increased blurriness of printed words: Text, especially fine print, might become nearly impossible to read without magnification.
- Diminished brightness of colors: Colors might seem consistently muted or dull.
- Difficulty recognizing people’s faces: Familiar faces might become hard to identify unless they’re very close.
- Increased blind spot in central vision: This blind spot might grow over time, making central vision tasks (like reading) increasingly difficult.
Diagnostic Methods
Diagnosis of AMD often involves a combination of methods:
Eye examination
A comprehensive exam where an ophthalmologist checks for drusen (tiny yellowish deposits that form under the retina) or any pigmentation changes indicative of AMD.
Optical coherence tomography (OCT)
A non-invasive imaging test, OCT captures cross-sectional images of the retina, allowing the doctor to measure its thickness and identify swelling or fluid under the retina.
Fluorescein angiography
In this test, a fluorescent dye is injected into the arm. A camera captures the dye’s journey through the blood vessels in the eye, highlighting any leaking vessels.
Amsler Grid
This is a simple test where the patient looks at straight lines on a grid. Distortions or breaks in these lines might indicate the presence of macular degeneration.
Regular eye check-ups, especially for those over 50 or with risk factors, are crucial for early detection and management of AMD.
Treatment and management
Macular degeneration, particularly the wet form, requires vigilant management to help preserve vision. While there is no outright cure, various AMD treatments and strategies can slow its progression and help patients manage their symptoms more effectively.
It’s essential to understand that while treatments can help manage the condition and improve life quality, they do not cure macular degeneration. The primary aim is to stabilize vision and, where possible, regain some lost sight.
Treatment options for wet AMD
Injections
Anti-VEGF (Vascular Endothelial Growth Factor) drugs, such as ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin), can be injected into the eye. They help counteract the growth of new, abnormal blood vessels and reduce the leaking that can cause rapid and severe vision loss.
💡 Read more: What Happens if You Stop Taking Eye Injections for Macular Degeneration?
Lazer therapy
There are two main types:
- Photodynamic Lazer Therapy: A two-step treatment in which a light-sensitive drug is used to damage the abnormal blood vessels.
- Lazer Photocoagulation: Directly targets and destroys leaking vessels but can also damage surrounding tissue.

Prevention
While AMD’s onset is influenced by genetics and age, several preventive measures can help reduce the risk or slow its progression.
Importance of Early Detection
Recognising early symptoms and seeking prompt medical advice can lead to timely interventions, potentially slowing the progression and minimizing vision loss.
Lifestyle Changes
Adopting certain lifestyle changes can play a crucial role in the management and prevention of AMD’s progression. Not only do these changes reduce the risk of AMD but they also promote overall eye health and general well-being.
1. Balanced diet
A diet rich in specific nutrients can potentially slow the progression of AMD and enhance overall eye health:
- Antioxidants: These help combat free radicals in the body, which can damage the macula. Sources include:
– Vitamin C: Citrus fruits, strawberries, bell peppers, and broccoli.
– Vitamin E: Nuts, seeds, spinach, and broccoli.
– Beta-carotene: Carrots, sweet potatoes, and kale. - Lutein & Zeaxanthin: These carotenoids are found in high concentrations in the macula and help protect it from harmful light effects. Incorporate foods like:
– Kale, spinach, and other leafy greens.
– Eggs, corn, and orange bell peppers. - Omega-3 Fatty Acids: Beneficial for retinal function and may reduce the risk of chronic diseases. Sources include:
– Fatty fish like salmon, mackerel, and sardines.
– Walnuts, flaxseed, and chia seeds.
💡 More information: What Foods Should Be Avoided With Macular Degeneration?
2. No smoking
The harmful effects of smoking extend beyond the lungs and heart to the eyes:
- Accelerated Risk: Smoking has been shown to double the risk of AMD. It introduces harmful chemicals into the bloodstream that can damage the eyes and reduce the blood’s oxygen-carrying capacity, crucial for retinal health.
- Progression: Smokers might experience faster progression of AMD compared to non-smokers.
- Cease Smoking: Quitting smoking, regardless of how long one has smoked, can reduce the risk of AMD progression. Various resources, including counseling, medications, and support groups, can aid in the quitting process.
3. UV protection
Shielding eyes from harmful UV rays is essential in the prevention of eye conditions:
- Damage from UV Rays: Prolonged exposure to UV rays can accelerate macular damage and may contribute to cataract formation.
- Protection: It’s crucial to wear sunglasses that block 100% of UVA and UVB rays. This can protect the eyes from direct and reflected sunlight, particularly useful in water, snow, or sand environments.
- Additional Measures: Wearing wide-brimmed hats or caps can further reduce the amount of UV exposure, especially during peak sunlight hours.
Low vision aids and rehabilitation
These are specialized tools and training strategies to help patients maximize their remaining vision and maintain independence. Examples include magnifying glasses, screen readers, and large-print books.
💡 Read more: What Are the Best Glasses for Macular Degeneration?
Regular eye check-ups
Routine eye examinations, especially for those in high-risk categories, can detect changes early. This proactive approach can lead to timely interventions, which can be crucial for preserving vision.
Supplements
Dietary supplements containing a specific mix of vitamins and minerals can reduce the risk of AMD progression. The AREDS2 supplements, for instance, have been linked to a reduced risk of advanced AMD. Products like Eyesight Plus can also help maintain eyesight and fight AMD by providing essential ingredients supportive of eye health. However, always consult with an ophthalmologist before starting any supplementation regimen.
In essence, while macular degeneration poses a challenge, an amalgamation of medical treatments, lifestyle changes, and preventive measures can significantly impact an individual’s ability to manage and live with the condition.
Early prevention and detection is key
In understanding macular degeneration, we recognise the fragility of our central vision and the significance of the macula. Though this condition poses challenges, early detection, treatments, and supportive measures, such as Eyesight Plus, can play pivotal roles in preserving eye health. Staying informed and proactive ensures a brighter, clearer future for our vision.

Frequently asked questions
- What is the main cause of macular degeneration?
Macular degeneration is primarily caused by aging and genetic factors. Over time, the tissues in the retina and macula can deteriorate, leading to AMD. Family history also plays a significant role, and several genes have been linked to a higher risk of developing the condition.
- Can macular degeneration lead to complete blindness?
While macular degeneration can lead to significant vision loss, it usually does not cause total blindness. It primarily affects central vision, which means individuals might still retain peripheral vision. However, the loss of central vision can significantly impair tasks like reading, driving, and recognising faces.
You may want to read: What does vision look like with macular degeneration?
- Is there any cure for macular degeneration?
Currently, there is no outright cure for macular degeneration. However, treatments and management strategies are available to slow its progression and help manage the symptoms.
- How is macular degeneration diagnosed?
Diagnosis typically involves a comprehensive eye examination, including tests like optical coherence tomography (OCT) and fluorescein angiography. The Amsler Grid, a simple visual tool, can also help detect changes in vision that might indicate the presence of macular degeneration.
- What are the available treatments for wet macular degeneration?
Wet AMD can be treated with anti-VEGF injections that counteract the growth of new, abnormal blood vessels. Laser therapies, including photodynamic laser therapy and laser photocoagulation, can also be effective.
- Can I prevent macular degeneration with diet and lifestyle changes?
While you can’t entirely prevent AMD, certain lifestyle modifications can reduce the risk or slow its progression. You may wonder how long it takes to lose vision with AMD, and it depends entirely on its progression and your lifestyle. Improving your diet and lifestyle include maintaining a diet rich in antioxidants and omega-3s, regular exercise, ceasing smoking, and protecting the eyes from excessive UV exposure.
- What resources are available for individuals living with macular degeneration?
Several organizations and groups provide resources and support for those with AMD. This includes the Macular Society in the UK, which offers guidance, support groups, and up-to-date research findings. Additionally, low-vision clinics and rehabilitation services can offer tools and strategies to help maximize remaining vision.
- Are supplements beneficial in managing or preventing macular degeneration?
There are natural ways of healing macular degeneration, and taking supplements is a beneficial way of doing this. Certain dietary supplements, like the AREDS2 supplements, have been shown to reduce the risk of AMD progression. Eyesight Plus, for example, includes essential ingredients that can help maintain eyesight and improve eye health. However, it’s crucial to consult an ophthalmologist before starting any supplementation.
Understanding AMD, its causes, and potential treatments can offer hope and direction for those affected and their loved ones. If you suspect you’re at risk or notice vision changes, always seek advice from a healthcare professional.